Tag: TMJ dysfunction
14 Posts


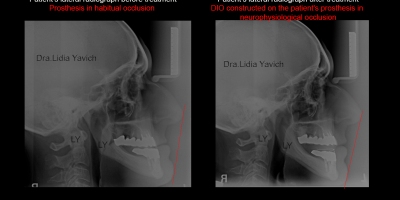
Posteriorization of the Mandibular Condyle, Compression of the Retrodiscal Tissue and Anteriorization of the Articular Disc as a cause of Neurologic Pain. Recovery of the Physiological Relationship of the Head of the Mandible with the Articular Disc. Series of clinical cases.

Treatment of TMJ Pathologies: Patient with headache and excessive clenching. Physiological Neuromuscular Rehabilitation. First and second phase. Case Report.

The temporomandibular joint (TMJ) as a peripheral trigger in the headache. Physiological Neuromuscular Rehabilitation. First and second phase. Case Report.

TMJ Study and Investigation Page. Three years of publication.

TMJ Pathology in Professional Musicians: A look beyond the risk factors. Physiological Neuromuscular Rehabilitation. First and second phase. Case Report.
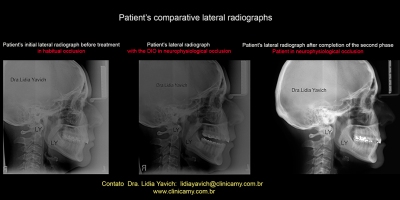
Neuromuscular Physiological Treatment in a Patient with Headache and Pain in the Temporomandibular Joints. Case report without possibility of Disc Recapture: first and second phase.
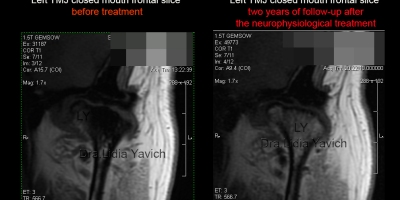
Reestablishment of the Bone Marrow Signal in a case of Avascular Necrosis of the Mandibular Head. Monitoring two years after treatment.

Temporomandibular Joint Pathology in a Patient with Congenital Fusion of two Cervical Vertebrae. First and Second Phase. Case Report.