Female patient, 40 years old comes to consultation referred by her rheumatologist WITH STRONG PAIN IN the TMJ (temporomandibular joint), TWINGES IN THE HEAD AND MOUTH OPENING LIMITATION.
The patient had a diagnosis of seronegative spondyloarthropathy until then nonspecific.Later diagnosed as Ankylosing Spondylitis
Seronegative spondyloarthropathies refers to a group of diseases that share common characteristics, including the occurrence of inflammation in the spine, peripheral joints and in various peri-articular tissues, in particular entheses.
Seronegative spondyloarthropathies laboratory outstanding feature is the absence of rheumatoid factor and auto antibodies. They have strong association with human leukocyte antigen HLA-B27.
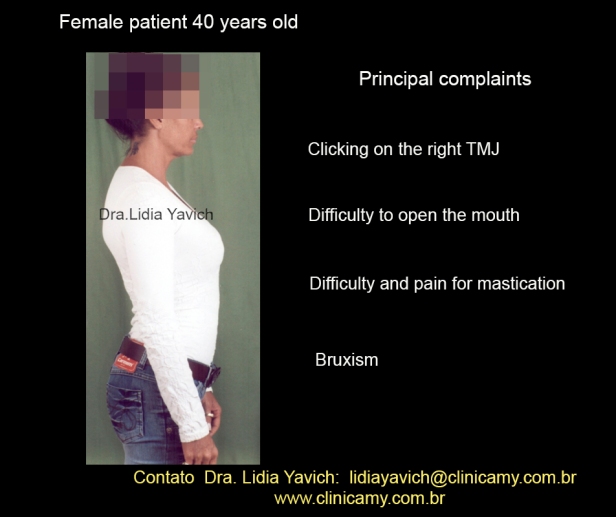
 The patient reports clicking on the right TMJ, difficulty to open the mouth, difficulty and paint in chewing. She also reports bruxism.
The patient reports clicking on the right TMJ, difficulty to open the mouth, difficulty and paint in chewing. She also reports bruxism.
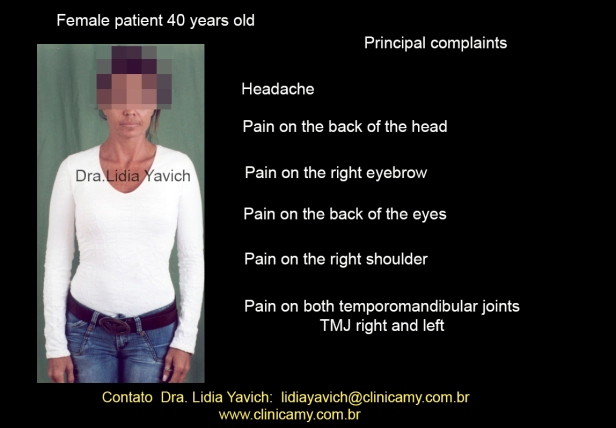
 She reports feeling headache, neck pain, pain in the right eyebrow, pain behind the eyes, pain in the right shoulder. She also reports pain in both temporomandibular joints which is stronger in the right joint.
She reports feeling headache, neck pain, pain in the right eyebrow, pain behind the eyes, pain in the right shoulder. She also reports pain in both temporomandibular joints which is stronger in the right joint.

The patient marks on the record the most important points of pain. In the first consultation, during the anamnesis the patient reported that she had initiated a treatment for the bruxism problem, and that at one point with the device change she began to feel a very strong pain and her mouth locked.
In the first consultation, during the anamnesis the patient reported that she had initiated a treatment for the bruxism problem, and that at one point with the device change she began to feel a very strong pain and her mouth locked.
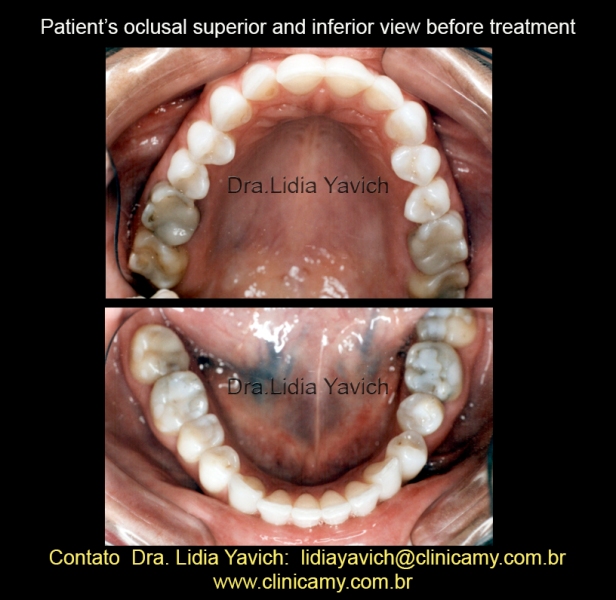 The occlusal view shows the superior anterior sector wear and the anterior lower sector wear.
The occlusal view shows the superior anterior sector wear and the anterior lower sector wear.
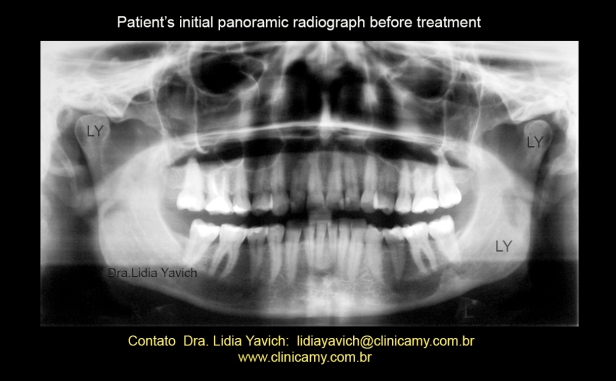 Patient’s panoramic radiograph.
Patient’s panoramic radiograph.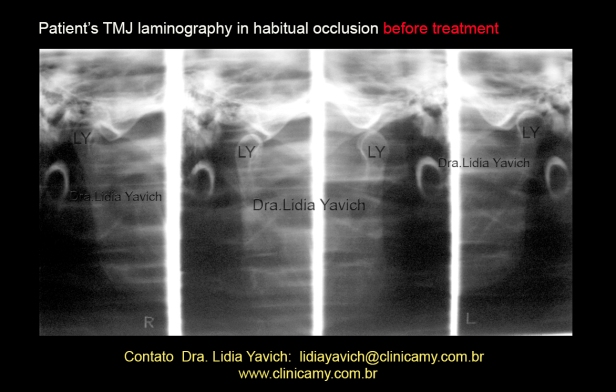 The joints radiographic image shows the superior and posterior positioning of the articular process on the left side in the joint cavity when the jaw is in maximal intercuspal position.
The joints radiographic image shows the superior and posterior positioning of the articular process on the left side in the joint cavity when the jaw is in maximal intercuspal position.
In the maximum opening position, there is flattening of the posterior and anterior surface of the left mandibular condyle process and a flattening of the superior and anterior surface of the right mandibular condyle process. The right side also presents an alteration of the growth axis of the mandibular condyle.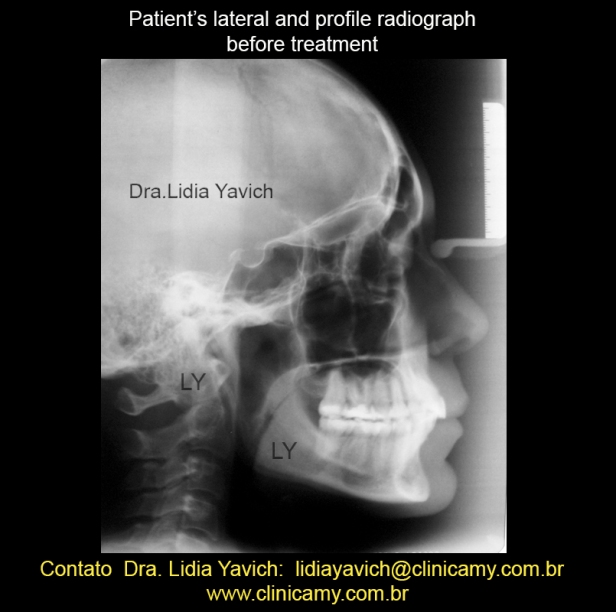 Patient’s lateral and profile radiograph before treatment.
Patient’s lateral and profile radiograph before treatment.
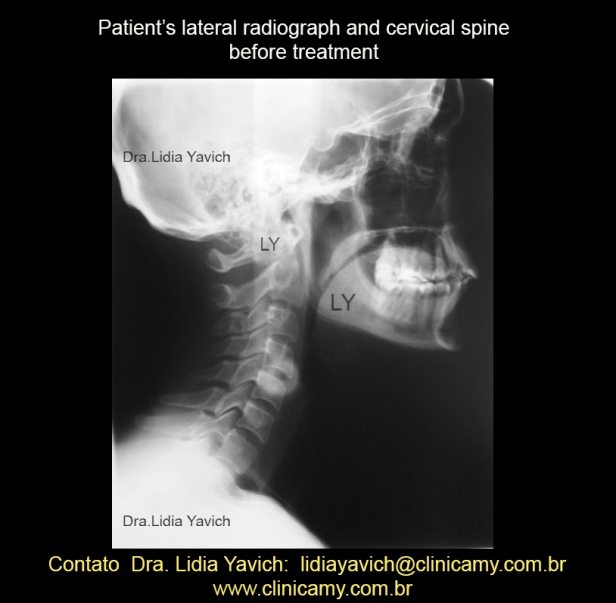 Patient’s lateral radiograph and cervical spine before treatment.
Patient’s lateral radiograph and cervical spine before treatment.
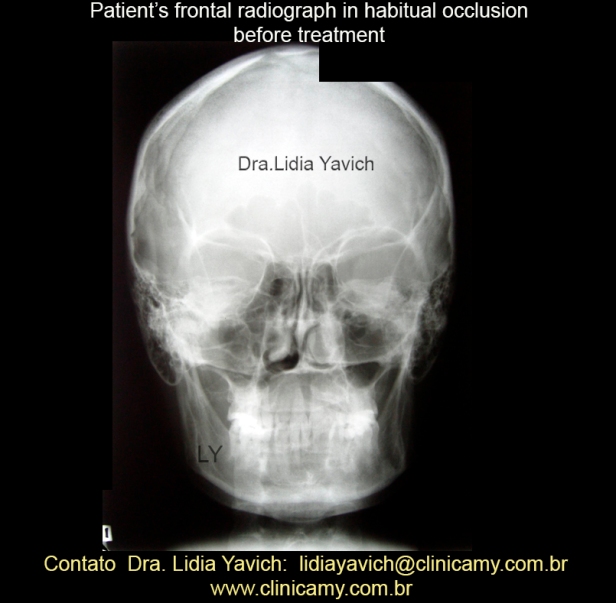 Patient’s frontal radiograph in habitual occlusion before treatment.
Patient’s frontal radiograph in habitual occlusion before treatment.
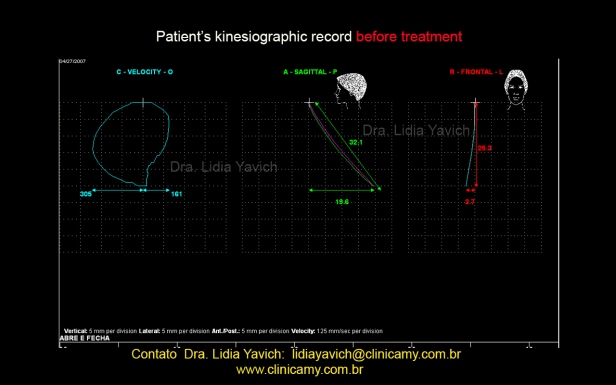 Opening and closing computerized kinesiographic record, the patient can open only 32 mm feeling strong pain, which shows an important limitation.
Opening and closing computerized kinesiographic record, the patient can open only 32 mm feeling strong pain, which shows an important limitation.
The patient also has a deflection of 2.7 mm to the right.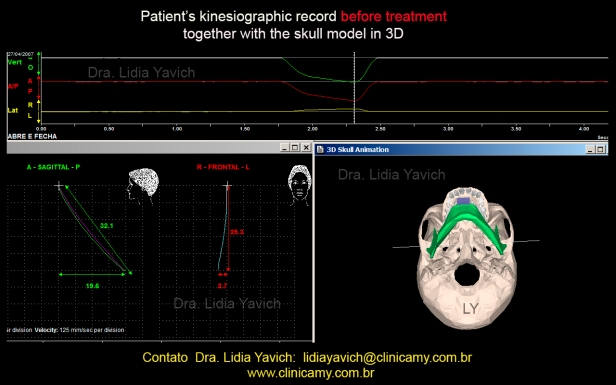 Note in the skull graph, the left condyle moves more than the right condyle where the deviation is.
Note in the skull graph, the left condyle moves more than the right condyle where the deviation is.
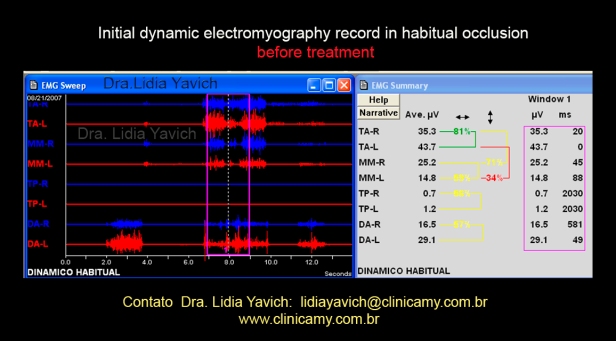 The surface electromyography exam evaluates the superior anterior temporal right and left, the right and left masseter, the right and left digastrics and the right and left upper trapezius.
The surface electromyography exam evaluates the superior anterior temporal right and left, the right and left masseter, the right and left digastrics and the right and left upper trapezius.
In this electromyography record the patient could not generate a good activity when we asked to bite hard (keeping the teeth in maximum intercuspation) and clench.
At the beginning of the record when we asked the patient to open the mouth it is important to note the different activity between right and left digastrics.
The left digastric activates double than the right digastric.
Image enlargement showing the difference in translation of the mandibular condyles. Patient in maximum mouth opening.
It is important to be able to understand and connect all the information, the surface electromyography and the computerized kinesiograph. These data still does NOT PROVIDE A DIAGNOSIS, However they are tools to help us in the diagnosis.
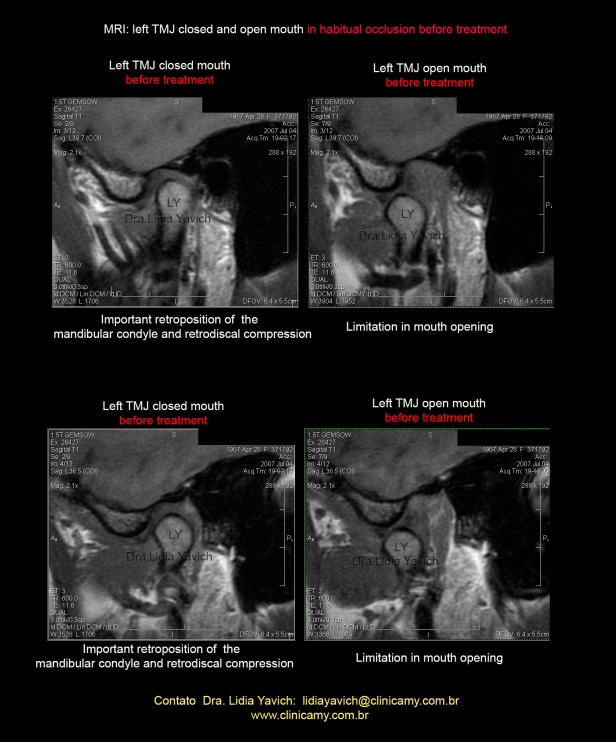
I asked the patient for an MRI-(magnetic resonance imaging) of the temporomandibular joints.
When the patient filled out the clinical record for the MRI she reported that she did a tattoo a month before, that prevented the realization of the MRI until completing the time of three months after the realization of the tattoo.
Remember that the resonator is a large magnet and tattoos have pigments which may contain metal and could heat up and cause burns.
We kept the patient with a temporary splint until we had the MRI information, as explained in previous posts; WE MUST NOT TREAT A PATIENT WITHOUT A DEFINED DIAGNOSIS.
We could easily assume that as the patient had a systemic nonspecific inflammatory arthritis attacking various joints of her body also the TMJ could be involved.
It is fundamental to rethink something which SOMETIMES could be ONLY A CONJECTURE, even if the patient is a carrier of an inflammatory autoimmune disease.
In the systemic part it is the rheumatologist who will decide the therapy.
Our part is to promote a non-compressive position of the TMJ where the masticatory muscles may perform without loading the joint, and where the patient can fulfill all the functions of the stomatognathic system.
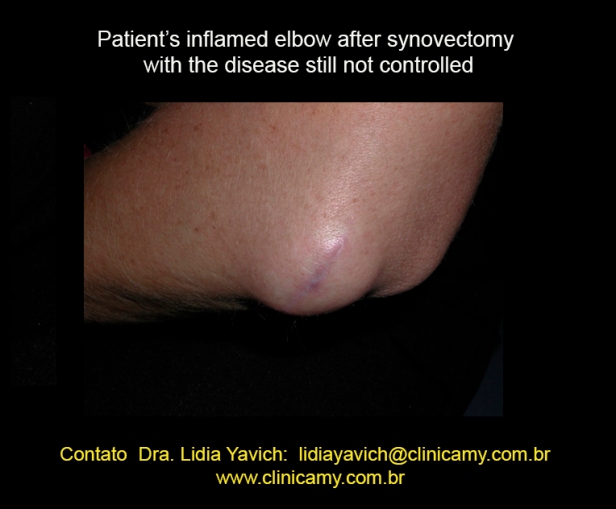 Patient’s inflamed elbow after synovectomy with the disease still not controlled
Patient’s inflamed elbow after synovectomy with the disease still not controlled
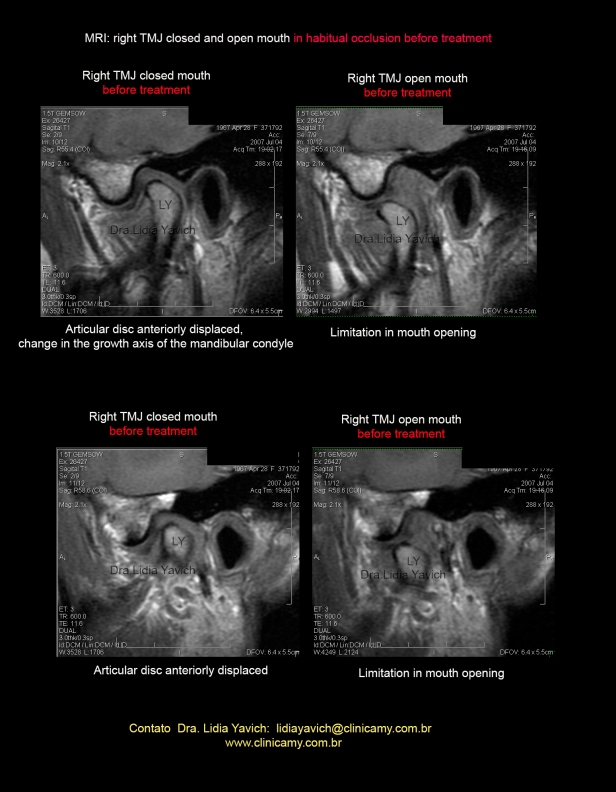 MRI: sagittal sections selected. Left TMJ closed mouth: articular disc anteriorly displaced. Change in the growth axis of the mandibular condyle.
MRI: sagittal sections selected. Left TMJ closed mouth: articular disc anteriorly displaced. Change in the growth axis of the mandibular condyle.
Left TMJ open mouth: limitation in mouth opening.
The images here are in T1, all images analyzed including T2 and STIR DOES NOT SHOW inflammatory signs.
It is relevant to remember that in the first consultation, during the anamnesis the patient reported that she had initiated a treatment for the bruxism problem, and that at one point with the device change she began to feel a very strong pain and the mouth locked.
The patient remembers that the device change aimed to align the median line of the upper incisors to the median line of the lower incisors.
This has to be a warning to all of us in dentistry which were taught to carry out all our treatments without knowing the condition of the TMJ.
 MRI: sagittal sections selected. Right TMJ closed mouth: articular disc anteriorly displaced. Change in the growth axis of the mandibular condyle.
MRI: sagittal sections selected. Right TMJ closed mouth: articular disc anteriorly displaced. Change in the growth axis of the mandibular condyle.
Right TMJ open mouth: limitation in mouth opening.
After conducting the analysis of the MRI images, studying all the slices and all required parameters (not included in the post), we can proceed to carry out a neuromuscular physiologic record.
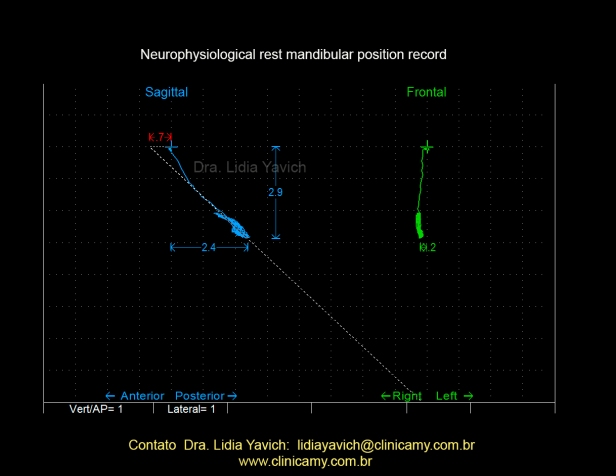 The masticatory muscles of the patient were electronically deprogrammed and the rest position was recorded with a computerized kinesiograph.
The masticatory muscles of the patient were electronically deprogrammed and the rest position was recorded with a computerized kinesiograph.
This record has been difficult to achieve. The patient was limited and in great pain. A very low DIO was made, leaving an interocclusal free space of one mm which would normally be too little.
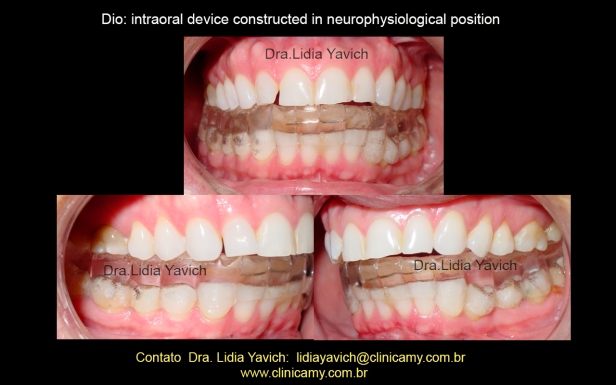 DIO (intraoral device constructed in neurophysiologic position)
DIO (intraoral device constructed in neurophysiologic position)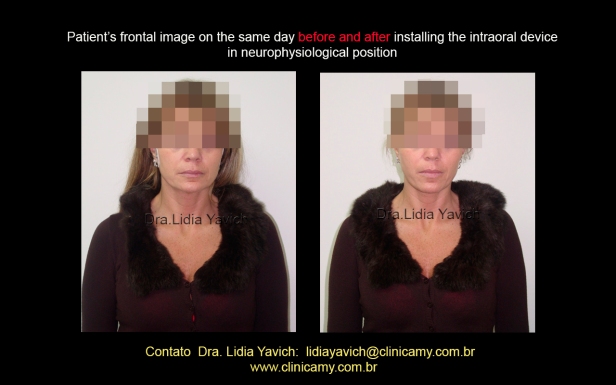 Patient’s frontal image on the same day, before and after installing the intraoral device in neuromuscular physiologic position.
Patient’s frontal image on the same day, before and after installing the intraoral device in neuromuscular physiologic position.
 Patient’s lateral image on the same day, before and after installing the intraoral device in neuromuscular physiologic position.
Patient’s lateral image on the same day, before and after installing the intraoral device in neuromuscular physiologic position.
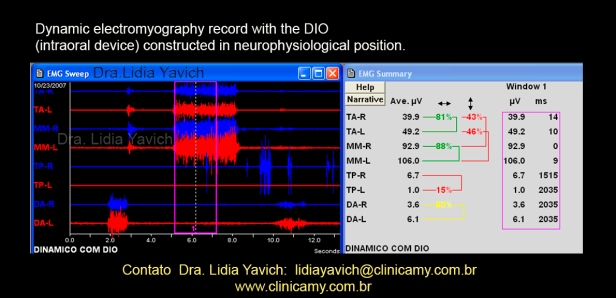 Patient’s electromyography record in neurophysiologic occlusion wearing the device (DIO), even the muscles activation is low the difference with the initial record is remarkable.
Patient’s electromyography record in neurophysiologic occlusion wearing the device (DIO), even the muscles activation is low the difference with the initial record is remarkable.
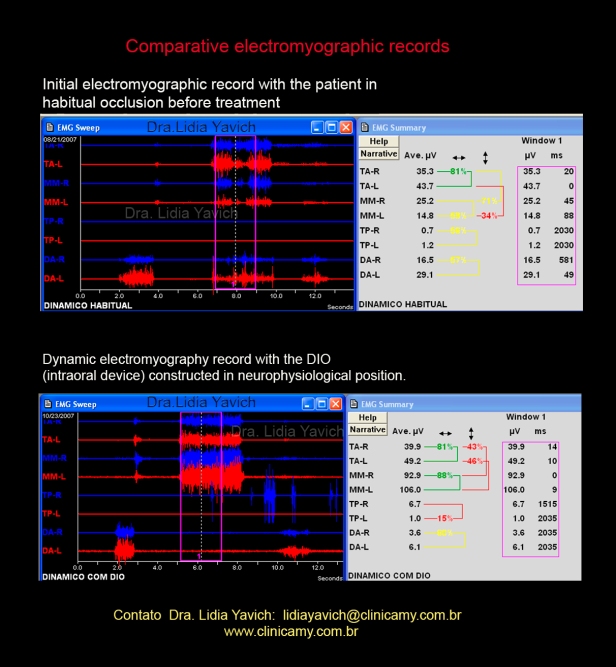 Comparative EMG records: the upper in habitual occlusion and lower in neurophysiological occlusion with the DIO (intraoral device).
Comparative EMG records: the upper in habitual occlusion and lower in neurophysiological occlusion with the DIO (intraoral device).
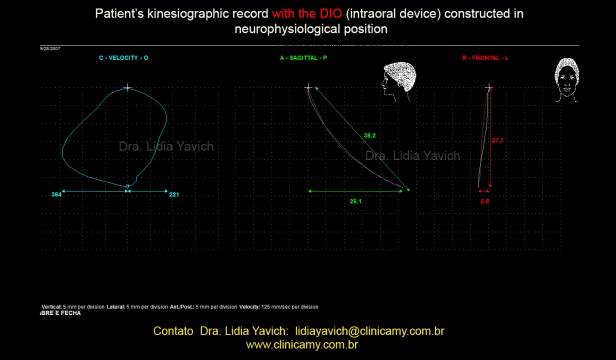 Patient’s kinesiographic record with the DIO (intraoral device) constructed in neurophysiological position.Improvement in mouth opening.
Patient’s kinesiographic record with the DIO (intraoral device) constructed in neurophysiological position.Improvement in mouth opening.
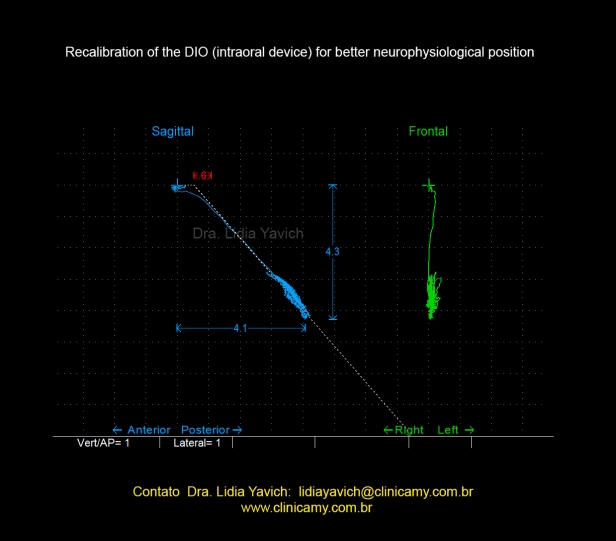 DIO recalibration to improve the patient’s neuromuscular physiological position. The condition of the patient now allows best records because the significant decrease in pain.
DIO recalibration to improve the patient’s neuromuscular physiological position. The condition of the patient now allows best records because the significant decrease in pain.
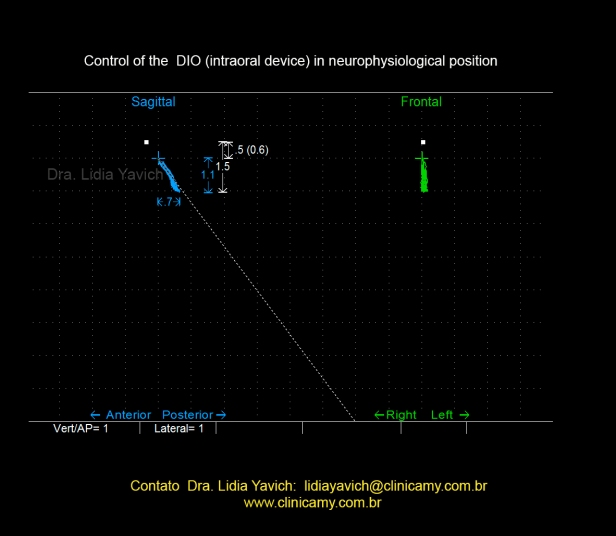 Control of the intraoral device, habitual and neuromuscular trajectory are coincident.
Control of the intraoral device, habitual and neuromuscular trajectory are coincident.
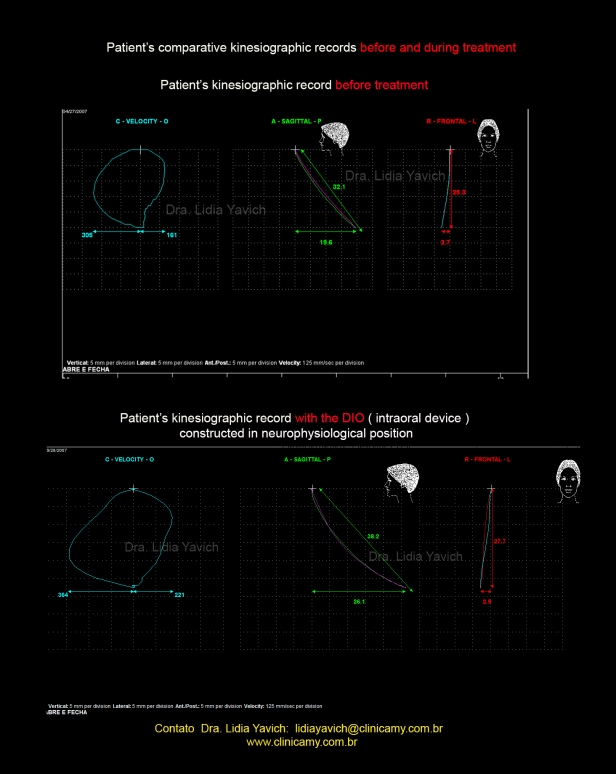 Patient’s comparative kinesiographic records before and during treatment. Improvement of the patient mandibular opening.
Patient’s comparative kinesiographic records before and during treatment. Improvement of the patient mandibular opening.
 Note on the skull graphic, both condyles right and left move symmetrically.
Note on the skull graphic, both condyles right and left move symmetrically.
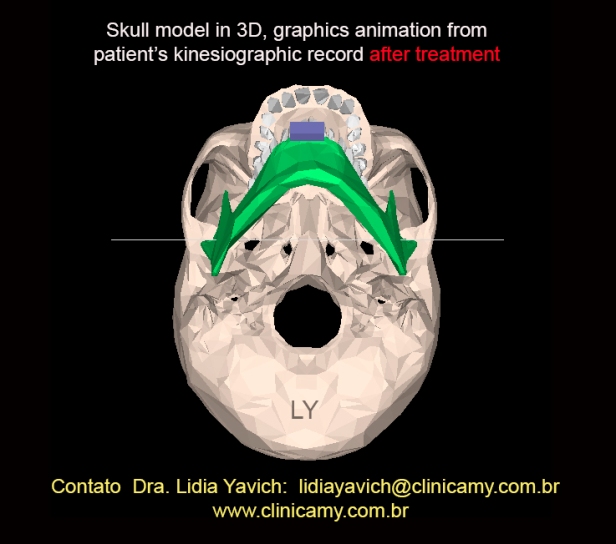 Image enlargement showing both condyles right and left moving symmetrically. Patient in maximum mouth opening.
Image enlargement showing both condyles right and left moving symmetrically. Patient in maximum mouth opening.
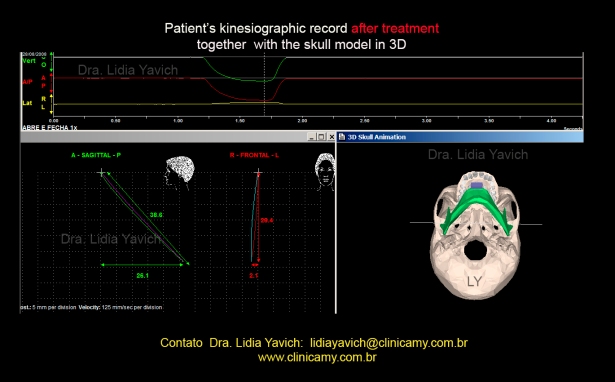
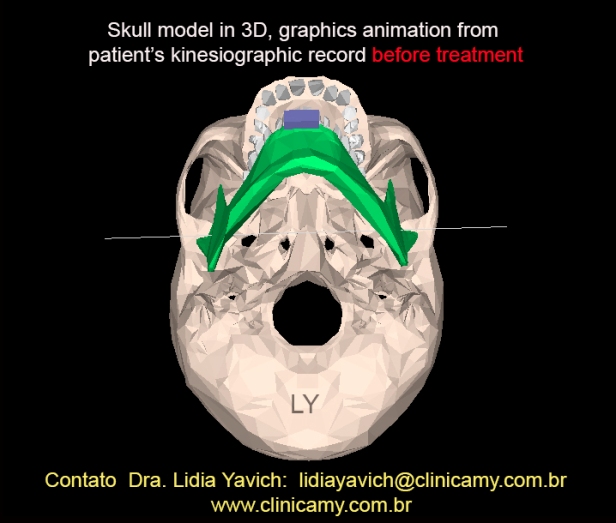
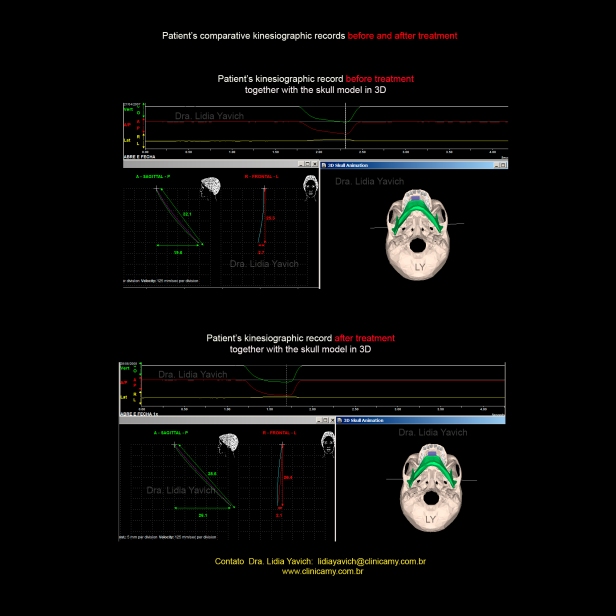 Patient’s kinesiographic records comparison with the skull 3D model before and after treatment.
Patient’s kinesiographic records comparison with the skull 3D model before and after treatment.
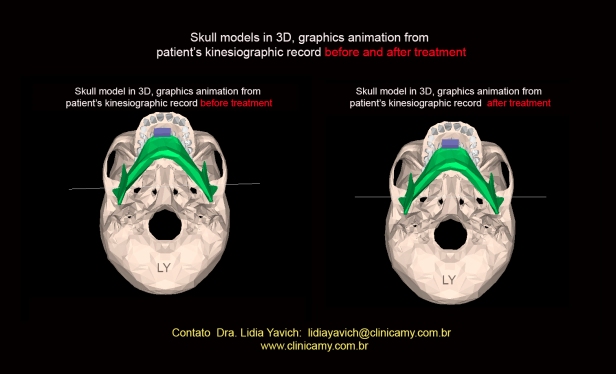 Skull models in 3 D, graphic animation from patient’s kinesiographic record before and after treatment comparison. Patient in maximum mouth opening.
Skull models in 3 D, graphic animation from patient’s kinesiographic record before and after treatment comparison. Patient in maximum mouth opening.
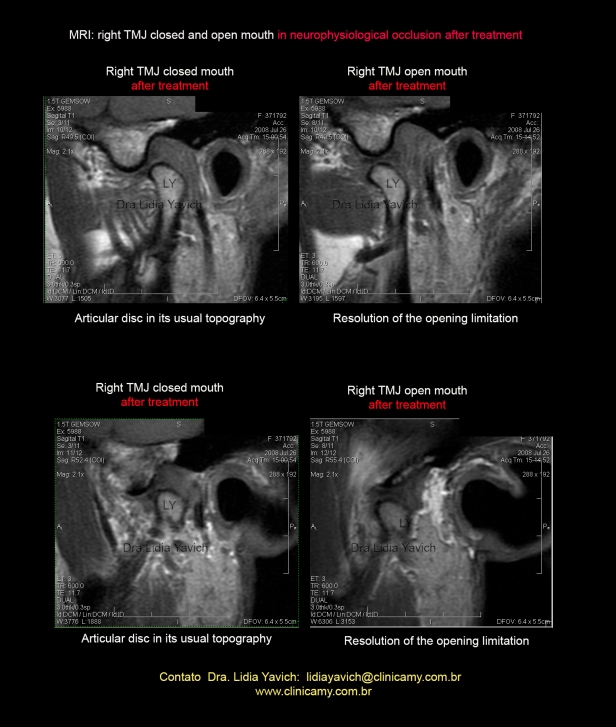 MRI: Right TMJ, closed and open mouth before and after treatment. Articular disc in habitual position,(the disc was dislocated before treatment) Resolution of the opening limitation.
MRI: Right TMJ, closed and open mouth before and after treatment. Articular disc in habitual position,(the disc was dislocated before treatment) Resolution of the opening limitation.
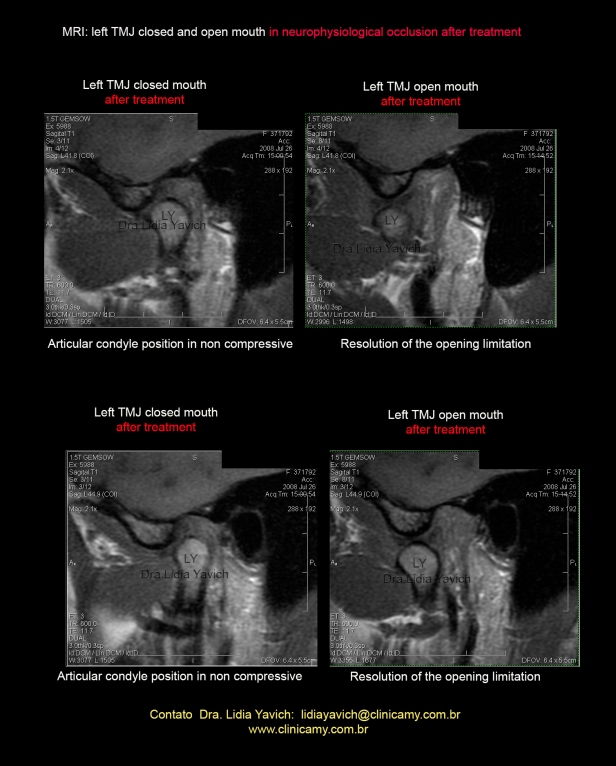 MRI: Leftt TMJ, closed and open mouth before and after treatment. Articular disc in habitual position. Resolution of the opening limitation.
MRI: Leftt TMJ, closed and open mouth before and after treatment. Articular disc in habitual position. Resolution of the opening limitation.
 MRI: TMJ sagittal comparative images, open and closed mouth before and after treatment.
MRI: TMJ sagittal comparative images, open and closed mouth before and after treatment.
 The patient without pain, decided to continue with the DIO and not perform the phase 2 to eliminate de DIO, with a tridimensional orthodontics.
The patient without pain, decided to continue with the DIO and not perform the phase 2 to eliminate de DIO, with a tridimensional orthodontics.
She decided only to restore the teeth that were worn. Restorations made by Dr. Luis Daniel Yavich Mattos.
When I was 39 years old I was diagnosed by my rheumatologist with arthritis.
All major joints of my left side were suddenly and without warning, very swollen, such as knee and elbow, preventing me from performing my simplier movements such as standing and stretching my arm.
I had swelling, redness and intense pain. Then I started to feel pain in the TMJ. I ended up in the clinic of an orthodontist and facial orthopedist who told me that I had ‘bruxism’ and that I needed to use a device to place the tongue in the right position.
I wore the appliance for a month or two, my TMJ locked, I could not open my mouth and I felt an absurd pain in my entire head, I no longer knew what hurted more, if it were the joints of the body or my head and mouth.
My rheumatologist, apprehensive that I could have arthritis also in the TMJ immediately referred me to Dr. Lidia Yavich, who received me in the office and managed to relieve my pain completely .
I HAVE TO STRESS THAT, THERE WAS NO MEDICATION THAT COULD CEASE THE PAIN that I felt in the TMJ and in the cervical spine, NOTHING!
After the imaging studies performed by indication of Dr. Lidia, we came to the conclusion that I was not suffering from arthritis in both TMJ, but from a dislocation of my right condyle after using for a short time a mistaken device to place my bite and tongue in the ” RIGHT POSITION”
That treatment did not considered important assumptions as the asymmetry of my condyles, or their position, or the disc status in relation to the condyles, causing much suffering.
It took me a long time to understand what was happening to me in my TMJ; I suffered from absurd pain in the head in the middle of a very difficult treatment for arthritis. I was disfigured, terrified and unsure after using the first device with the previous professional because he did not know how to end the pain and even seemed, not to know what was actually happening with me.
I had panic to imagine that I had arthritis in my TMJ, but only after the MRI and the Dr. Lidia interpretation it was possible to exclude the possibility of rheumatic disease in the TMJ in that moment, and from then on to make an efficient treatment.
In a few weeks Dr. Lidia not only took out ALL THE PAIN of the TMJ, but also led me to a treatment that repositioned my disc and stopped the pain, even being a carrier of a severe autoimmune disease.
I have been using the DIO for seven years without any pain, I have full understanding of the meaning of bruxism in my case and correct approach to the problem, including the options that I could have for a more permanent solution instead the use of the DIO.
I am very grateful to my rheumatologist today for indicating me a treatment that saved me, because I certainly would have gone crazy with those TMJ pains.
I am very grateful to Dr. Lidia who took me from the rock bottom in which I found myself, ignorant from all that was happening in a joint so unknown from most of us:.the TMJ.

Congratulations for the excellent paper. Thanks for sharing it.
Gianfranco Albergo
LikeLike
Thank you Gianfranco Albergo.
LikeLike